A number of groundbreaking and practice-changing studies were presented at the San Antonio Breast Cancer Symposium 2020.
The RxPONDER, ADAPT, and PRIME-2 trials revealed patients who can forgo chemotherapy or radiotherapy, monarchE and PENELOPE-B showed conflicting results with CDK4/6 inhibitors, one study indicated that a new tool can guide adjuvant chemotherapy, and another study suggested that circulating tumor cells (CTCs) can predict overall survival (OS).
Alan P. Lyss, MD, subprincipal investigator for Heartland Cancer Research NCORP, joined host David H. Henry, MD, to discuss these and other studies — their top 10 presentations from SABCS 2020 — in this episode.
1. Abstract GS3-07. Identifying patients whose symptoms are under-recognized during breast radiotherapy: Comparison of patient and physician reports of toxicity in a multicenter cohort. https://bit.ly/2MGCVEH
- This presentation could be one of the most important stories to emerge from SABCS 2020, according to Dr. Lyss.
- The trial included 9,868 breast cancer patients who received radiotherapy over an 8-year period.
- Investigators compared patient and physician reports of toxicity during radiotherapy, assessing four symptoms: pain, pruritus, edema, and fatigue.
- Physicians under-recognized moderate to severe pain 30.9% of the time, pruritus 36.7% of the time, edema 51.4% of the time, and fatigue 18.8% of the time.
- “The bottom line is: We’ve got to do better at this, and the first step in correcting it is to acknowledge that there is a problem. This abstract established that,” Dr. Lyss said.
2. Abstract GS2-03. Prime 2 randomised trial (postoperative radiotherapy in minimum-risk elderly): Wide local excision and adjuvant hormonal therapy +/- whole breast irradiation in women =/> 65 years with early invasive breast cancer: 10-year results. https://bit.ly/3omINAL
- The trial enrolled 1,326 women with histologically confirmed, unilateral invasive, hormone receptor-positive (HR+) breast cancer who were all 65 or older, had a tumor measuring 3 cm or less, had no nodal involvement, and were about to undergo breast-conserving surgery.
- The women were randomized 1:1 to receive adjuvant whole-breast irradiation or no radiotherapy in addition to adjuvant endocrine therapy.
- At 10 years, the rate of ipsilateral recurrence was significantly lower with radiotherapy than without it (0.9% vs 9.8%, P = .00008). The 10-year rate of regional recurrence was significantly lower with radiotherapy as well (0.5% vs. 2.3%, P = .014).
- There was no significant difference in the radiotherapy and no-radiotherapy arms when it came to distant recurrence (3.6% vs. 1.9%, P = .07), contralateral recurrence (2.2% vs. 1.2%, P = .20), non–breast cancer (8.7% vs. 10.2%, P = .41), metastasis-free survival (96.4% vs. 98.1%, P = .28), or OS (81.0% vs. 80.4%, P = .68).
- These results suggest radiotherapy could be omitted in this patient population, but the decision should be discussed and tailored to the individual patient, according to Dr. Henry.
3. Abstract GS1-01. Primary outcome analysis of invasive disease-free survival for monarchE: abemaciclib combined with adjuvant endocrine therapy for high-risk early breast cancer. https://bit.ly/38oSHwt
- The monarchE trial enrolled 5,637 women with HR+, HER2- early breast cancer.
- Cohort 1 included patients with four or more positive nodes, up to three positive nodes and a tumor size ≥ 5 cm, or grade 3 disease.
- Cohort 2 included women with up to three positive nodes and a Ki-67 index ≥ 20%.
- Patients in both cohorts were randomized to standard endocrine therapy alone or standard endocrine therapy with abemaciclib.
- The 2-year rate of invasive disease-free survival (IDFS) was 92.3% in the abemaciclib arm and 89.3% in the control arm (P = .0009). The 2-year distant relapse-free survival rate was 93.8% and 90.8%, respectively (P = .0009).
- Dr. Lyss said this is the first real advance in HR+ breast cancer adjuvant treatment in many years and has the potential to save thousands of lives. However, these are early data and should be interpreted with caution.
4. Abstract GS1-02. Phase III study of palbociclib combined with endocrine therapy (ET) in patients with hormone-receptor-positive (HR+), HER2-negative primary breast cancer and with high relapse risk after neoadjuvant chemotherapy (NACT): First results from PENELOPE-B. https://bit.ly/2XeQvRs
- The PENELOPE-B trial enrolled 1,250 women who had completed neoadjuvant chemotherapy and locoregional therapy.
- They were randomized to palbociclib plus endocrine therapy or endocrine therapy plus placebo.
- There was no significant difference in IDFS with palbociclib or placebo at 2 years (88.3% vs. 84%), 3 years (81.2% vs. 77.7%), or 4 years (73% vs. 72.4%).
5. Abstract GS4-10. Development and validation of a tool integrating the 21-gene recurrence score and clinicopathologic features to individualize prognosis for distant recurrence and prediction of absolute chemotherapy benefit in early breast cancer. https://bit.ly/38htoMD
- The RSClin tool integrates the 21-gene recurrence score and clinicopathologic features, including the grade of the tumor, the tumor size, and the patient's age.
- Researchers found that RSClin could guide adjuvant chemotherapy in HR+, HER2-, axillary node-negative breast cancer with greater precision, when compared with clinicopathologic features or genomic data alone.
- RSClin is available at https://online.genomichealth.com/.
6. Abstract GS4-08. Clinical utility of repeated circulating tumor cell (CTC) enumeration as early treatment monitoring tool in metastatic breast cancer (MBC) - a global pooled analysis with individual patient data. https://bit.ly/2MGUrZp
- This study included 4,079 metastatic breast cancer patients who had undergone baseline and follow-up CTC measurements in previous trials.
- The investigators analyzed changes in CTC levels between baseline and follow-up to determine whether those levels were associated with OS.
- The median OS was 47 months for patients who were CTC-negative at both baseline and follow-up, 32.2 months for patients who were positive at baseline and negative at follow-up, 29.6 months for patients who were negative at baseline and positive at follow-up, and 17.8 months for patients who were positive at both time points.
- With the negative-negative group as the reference, hazard ratios were 1.52 for the positive-negative group, 1.74 for the negative-positive group, and 3.15 for the positive-positive group (P < .0001 for all).
7. Abstract GS3-00. First results from a phase III randomized clinical trial of standard adjuvant endocrine therapy (ET) +/- chemotherapy (CT) in patients (pts) with 1-3 positive nodes, hormone receptor-positive (HR+) and HER2-negative (HER2-) breast cancer (BC) with recurrence score (RS) < 25: SWOG S1007 (RxPonder). https://bit.ly/35bK7Px
- RxPONDER included 5,083 adults with HR+, HER2- breast cancer, one to three positive nodes, no contraindications to taxane and/or anthracycline-based chemotherapy, and recurrence scores of 25 or below.
- Patients were randomized 1:1 to receive endocrine therapy or chemo-endocrine therapy using three stratification factors: recurrence score (0-13 vs.14-25), menopausal status, and axillary nodal dissection vs. sentinel node biopsy.
- At a median follow-up of 5.1 years, there was no association between chemotherapy benefit and recurrence score values in the whole study population.
- In postmenopausal patients, there was no difference in 5-year IDFS between patients who received chemotherapy and those who didn’t (91.6% vs. 91.9%, P = .82).
- However, in premenopausal patients, the 5-year IDFS rate was 94.2% with chemotherapy and 89% without it (P = .0004).
- The data also showed an OS benefit with chemotherapy in premenopausal patients (P = .032), although this result is considered early due to few deaths at the time of evaluation.
- “These data really establish that postmenopausal women with between one to three involved nodes and an Oncotype DX score of 25 or less do not need post-operative adjuvant chemotherapy; end of discussion,” Dr. Lyss said. “For physicians who have been giving those women chemotherapy, these data are immediately practice- changing.”
8. Abstract GS4-04. Endocrine therapy alone in patients with intermediate or high-risk luminal early breast cancer (0-3 lymph nodes), Recurrence Score <26 and Ki67 response after preoperative endocrine therapy: Primary outcome results from the WSG-ADAPT HR+/HER2- trial. https://bit.ly/35edjVY
- In this phase 3 trial, researchers combined static biomarkers (recurrence score in baseline core biopsy) and dynamic biomarkers (Ki-67 response) in an attempt to optimize adjuvant therapy in luminal early breast cancer.
- The trial included 4,691 patients with HR+, HER2-negative, clinically high-risk disease who received about a month of standard endocrine therapy as neoadjuvant treatment.
- Patients with a pretreatment recurrence score of 0-11 continued endocrine therapy alone with no planned chemotherapy at all.
- Patients with a pretreatment recurrence score of 12-25 received their month of endocrine therapy and then had a core biopsy of their residual tumor. If the Ki-67 had dropped to less than 10%, the patient continued endocrine therapy alone. If the Ki-67 remained > 10% or the patient had clinical N2 or N3 lymph nodes, the patient was assigned to receive neoadjuvant chemotherapy.
- The 5-year IDFS rate was 92.6% in patients with a recurrence score of 12-25 and a Ki-67 response and 93.9% in patients with a recurrence score of 0-11.
- The 5-year distant relapse-free survival was 95.6% and 96.3%, respectively. The 5-year OS was 97.3% and 98%, respectively.
- These results suggest Oncotype DX testing could spare the majority of HR+, HER2- patients with zero to three positive lymph nodes from receiving chemotherapy, Dr. Lyss said.
9. Abstract GS3-01. Additional efficacy endpoints from the phase 3 KEYNOTE-355 study of pembrolizumab plus chemotherapy vs placebo plus chemotherapy as first-line therapy for locally recurrent inoperable or metastatic triple-negative breast cancer. https://bit.ly/394UCVX
- In KEYNOTE-355, 847 patients with locally recurrent, inoperable or metastatic triple-negative breast cancer were randomized to receive pembrolizumab plus chemotherapy or chemotherapy plus placebo. Chemotherapy consisted of nab-paclitaxel, paclitaxel, or gemcitabine plus carboplatin.
- The median progression-free survival (PFS) was longer in the pembrolizumab arm, at 7.5 months, versus 5.6 months with chemotherapy alone (hazard ratio, 0.82).
- The PFS was superior with pembrolizumab regardless of the chemotherapy partner.
- However, higher PD-L1 expression was associated with a longer PFS, a higher overall response rate, and a longer duration of response.
10. Abstract GS3-06. Biomarker evaluation in the phase 3 ASCENT study of sacituzumab govitecan versus chemotherapy in patients with metastatic triple-negative breast cancer. https://bit.ly/3hQ14nJ
- Trophoblast cell-surface antigen-2 (Trop-2) is highly expressed in triple-negative breast cancer.
- Sacituzumab govitecan (SG) consists of an anti-Trop-2 antibody coupled to SN-38, an active metabolite of irinotecan.
- In the ASCENT trial, patients with metastatic triple-negative breast cancer were randomized to SG or standard single-agent chemotherapy.
- A subgroup analysis of this trial showed that Trop-2 levels correlated with PFS and OS.
- Patients were divided into three groups by Trop-2 levels — low (H-score <100), medium (100-200), and high (200-300).
- In patients with low Trop-2 levels, the median PFS was 2.7 months with SG and 1.6 months without it. The median OS was 9.3 months and 7.6 months, respectively.
- In patients with medium Trop-2 levels, the median PFS was 5.6 months with SG and 2.2 months without it. The median OS was 14.9 months and 6.9 months, respectively.
- In patients with high Trop-2 levels, the median PFS was 6.9 months with SG and 2.5 months without it. The median OS was 14.2 months and 6.9 months, respectively.
*Some of the numbers mentioned in this episode are incorrect, but the correct numbers are reflected in the show notes. The data presented at SABCS 2020 sometimes differed from data included in the abstracts.
Disclosures:
Dr. Henry has no financial disclosures relevant to this episode.
Dr. Lyss writes a column for MDedge Hematology/Oncology called “Clinical Insights.” He has no other conflicts of interest.
* * *
For more MDedge Podcasts, go to mdedge.com/podcasts
Email the show: [email protected]
Interact with us on Twitter: @MDedgehemonc
David Henry on Twitter: @davidhenrymd
From The Podcast
Blood & Cancer
The official podcast feed of MDedge Hematology-Oncology, part of the Medscape Professional Network. On Thursdays, Dr. David Henry interviews key opinion leaders and rising stars in hematology and oncology. The information in this podcast is provided for informational and educational purposes only.Join Podchaser to...
- Rate podcasts and episodes
- Follow podcasts and creators
- Create podcast and episode lists
- & much more
Episode Tags
Claim and edit this page to your liking.
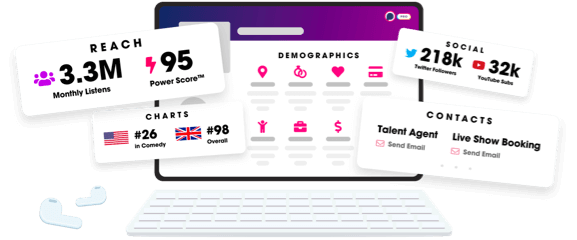
Unlock more with Podchaser Pro
- Audience Insights
- Contact Information
- Demographics
- Charts
- Sponsor History
- and More!
- Account
- Register
- Log In
- Find Friends
- Resources
- Help Center
- Blog
- API
Podchaser is the ultimate destination for podcast data, search, and discovery. Learn More
- © 2024 Podchaser, Inc.
- Privacy Policy
- Terms of Service
- Contact Us
