Dr. Shannon Westin and Dr. Mustafa Raoof discuss the paper "Medicare Advantage: A Disadvantage for Complex Cancer Surgery Patients."
TRANSCRIPT
Dr. Shannon Westin: Well, hello, everyone, and welcome back to another episode of the JCO After Hours podcast, where we get in-depth on articles that have been published in the JCO.
I am your host Shannon Westin, and it is my pleasure to serve as the Social Media Editor for the Journal of Clinical Oncology, as well as a Professor in GYN Oncology at The MD Anderson Cancer Center in Houston.
And today, I am very excited to be discussing a paper that was recently published in the JCO called “Medicare Advantage: A Disadvantage for Complex Cancer Surgery Patients.” And I am accompanied today by Dr. Mustafa Raoof, and he has no conflicts of interest to disclose. He is an Assistant Professor in the division of Surgical Oncology, Department of Surgery, and an Assistant Professor in the Department of Cancer Genetics and Epigenetics at the City of Hope Cancer Center. And there, he is a Surgical Oncologist with expertise in hepatobiliary and pancreatic cancer, and I'm thrilled to have him here today.
Welcome, Dr. Raoof.
Dr. Mustafa Raoof: Thank you. It's a pleasure to be here. Thank you for inviting me.
Dr. Shannon Westin: Of course. And thank you for your incredible work. We're going to get right to it. This is, I think, a really timely and important paper because I think we are always trying to understand how the insurance coverage or the medical coverage that our patients have here in the United States impacts their overall quality of care.
So, first, let's level set for the audience. Can you describe the basics of Medicare Advantage, which is what you explored in this paper, and how common is this coverage in the United States?
Dr. Mustafa Raoof: So, Medicare Advantage is the privatized aspect of Medicare, and what we know is that since the 1970s there were some private plans that were part of Medicare. But really at the turn of the century, 2000 and onwards, Medicare Advantage has gained a lot of popularity. And this is where the government basically pays a lump sum cost for a beneficiary to private insurance companies to manage Medicare. And so, it's a privatized product. And the idea there is that it's supposed to be an all-encompassing product for the beneficiaries, and the biggest advantage, initially at least, was that there was an out-of-pocket maximum, so patients are not subjected to extreme financial stresses.
The cost that was paid to Medicare Advantage plans per beneficiary were in the order of somewhere between 800 and $900 per beneficiary, per year. This was a little bit higher than what would have been the cost to Medicare, but that was to gain a lot of momentum into getting the private insurance interested in the plan. And then subsequently into that, there were a lot of incentives that were set for these Medicare Advantage plans based on some measures of quality, to kind of incentivize the quality products from this private insurance. And so, that's kind of the lay of the land for what the Medicare Advantage plans are.
Now, in terms of, how popular are they? I think this has grown significantly over the last 10 years, especially, 46% of all Medicare beneficiaries nationally are part of this Medicare Advantage plan, and it's not one plan, every private insurance company has their own offerings. But a significant majority, I think it's estimated that more than half, and even, you know, going beyond 10 years, the majority of Americans will be insured by these Medicare Advantage plans.
Dr. Shannon Westin: That's incredible, and certainly, that means this work that you did has such great impact with the number of patients that are going to be impacted. Can you give the listeners a little bit of an idea of how Medicare Advantage coverage might differ a little bit from the traditional? I know you mentioned the out-of-pocket costs, and that it's run by different companies, but any other kind of discerning features?
Dr. Mustafa Raoof: Yeah. So, with the Medicare Advantage plans, as I mentioned, you know, there's an out-of-pocket maximum. In addition, vision and dental plans, as well as gym memberships are included as part of the plan, to kind of provide a holistic plan to the older Americans. And then, one of the things that kind of stands out is that what is the downside to Medicare Advantage plans from a company that is providing this kind of a product, and so, they have to cut costs somewhere. So, I think the main downside to patients would be that their options, in terms of specialist care, will be limited because the networks are generally narrower. There is a variability in different plans as to how big and small their networks are, but they could be more restrictive, and if a potential beneficiary is not aware of that, they could lose out on seeing some doctors that they would've otherwise wanted to see.
Dr. Shannon Westin: Okay. That totally makes sense. And so, I guess the next natural question is, what led you to explore the impact of this coverage Medicare Advantage on patient outcomes in surgical practice?
Dr. Mustafa Raoof: Yeah. So, as somebody who sees patients with advanced cancer, I think a lot of Medicare Advantage beneficiaries are caught by surprise at the time when they're seeking out care, and they think that they have Medicare, and they should be able to seek whatever care that they would like. Whereas, you know, when they contact their provider, they're told that they have to go to a certain doctor in a certain network. And the shock that this is, as a secondary shock, in addition to the shock of a cancer diagnosis and needing a surgical intervention. So, early on in my training, I had seen some of that, and, you know, I really wanted to delve deeper into helper based problems, is: does it even matter if they go with different specialists, as long as there is some quality to that? And so, I started looking into the quality of the Medicare Advantage network from there on.
Dr. Shannon Westin: That leads us directly into your study. Why don't you give us a rundown of the design, and how you wanted to achieve those objectives that you just discussed?
Dr. Mustafa Raoof: So, leading up to the study, we had a publication in Annals of Surgery that looked at what do the networks look like for these Medicare Advantage plans. And that kind of information is hard to find. As you could tell, a lot of patients don't even know if a certain hospital will be covered by their insurance. And so, through a collaboration with Gretchen Jacobsen who studies this as well, they had compiled data on the networks for different hospitals, and for different plans in LA County, as to which hospitals were covered. So, we looked at that, and we found that a lot of these Medicare Advantage plans don't have access to high-volume hospitals, which was our way of measuring quality. And so, that kind of set the tone for this, and then we wanted to ask if there is a difference in outcome between patients who are insured by Medicare Advantage versus those who are insured by traditional Medicare.
Medicare Advantage data has been a little bit tricky to obtain for a lot of folks that I think it wasn't released because of data quality issues. We were a little bit lucky, in that we had access to the California Cancer Registry dataset, which includes all patients diagnosed with cancer in California, and that data was linked to discharge data from inpatient hospitalizations. And so, one of the categories that is collected is patients' insurance, whether it's Medicare or not, and whether it's managed or not. So, with that, we thought it was the perfect opportunity to ask a very simple question, and that question is, what are the differences in terms of access to high-volume surgery or quality cancer surgery, and what are the impacts on the outcome for the two different kinds of insurance plans?
So, the design is a retrospective cohort analysis, and we included all patients who were undergoing elective inpatient cancer surgery. We selected some index cancers, and we realized that it's not comprehensive, but we wanted to give it a go with some of the more common cancer diagnoses. So, we included lung, colon, and rectal, and then we also included some high complexity operations such as esophagus, stomach, pancreas, and liver, and we included all data from 2000 to 2020. And in terms of the primary objective of the study, we wanted to look at hospital mortality, so we looked at the association between 30-day hospital mortality, but we also looked at complications, readmissions, and failure to rescue. One of the other objectives of this study was to look at the association between insurance stipend, access to care-- we defined access to care in several different ways. Because there's no singular definition, we said access to care would be somebody getting access to cancer surgery at a Commission on Cancer-designated hospital, or NCI-designated cancer center, or a high-volume hospital, as defined by other authors previously, or a teaching hospital. So, we used several different definitions to kind of see if there is association between insurance and patients’ access to care.
Dr. Shannon Westin: And let's hear it. What were the results? How did Medicare Advantage compare to traditional Medicare?
Dr. Mustafa Raoof: Given our previous work on MA networks data, this was not a surprise, but when we saw that for all of the cancers that we looked at, there were significant barriers to access, in terms of getting to an NCI-designated cancer center, or a high-volume cancer center. So, no matter how we looked at it, we felt that there was a significant disparity in getting to these specialist hospitals, which we associate with quality of cancer surgery. But what was interesting in a major finding of the paper was that for certain cancers, for example, gastrectomy, pancreatectomy, and hepatectomy, we found significantly increased early-day mortality for those operations. And so, for example, for gastrectomy, there was 1.4-fold higher mortality, for pancreatectomy 1.9-fold, and then for hepatectomy, 1.4-fold. So, these are tangible figures in-- you know, the idea is that if somehow we can improve access to high-quality surgery within MA plans, to match that of traditional Medicare, which is not ideal still, but I think just by doing that, we could impact, potentially reduce cancer deaths from surgery itself.
Dr. Shannon Westin: So, I was struck by the fact that there was a difference between the outcomes you mentioned - stomach, pancreatic, liver surgery, and colon cancer. You know, why do you think there might be a difference?
Dr. Mustafa Raoof: That's a great question. So, I think colon cancer surgery has-- I wouldn't say it is low-complexity, but it's intermediate-complexity. And I think as a surgical workforce, a lot of surgeons who may or may not be trained with fellowship specialization, they are able to do a really good job of colon resection, and so, there are many high-volume surgeons that do not actually sit in NCI-designated cancer centers or CoC-accredited hospitals, and they're doing a really good job. And so, I think we see that the impact of access is less in colon surgery, and I think that may explain why that is.
Dr. Shannon Westin: We've looked at this, and I know you said that you picked some common cancers, and I know you did that because, you know, I'm a GYN Oncologist, so I was definitely interested in outcomes here. We definitely see that, in especially ovarian cancer surgery, which is rare, is that high-volume centers matter. And it can be a comprehensive cancer center, or it can just be a really high-volume center that draws a lot of ovarian cancer, it doesn't necessarily have to be a cancer center. So, that certainly makes a lot of sense. I guess the next question really is what happens next for this work? Like, what can we do to make a difference here?
Dr. Mustafa Raoof: So, just reading the landscape on health insurance, I think there's significant incentives for Medicare Advantage plans. So, I think that is going to exist, and I think that will be in the future. I think the important aspect will be to ensure the quality of Medicare Advantage plans. And I think the data that is presented in this study, we hope that it will shed some light, and give a voice to patients who are dealing with a situation where they need complex cancer surgery. And we also hope that there would be some transparency when patients are signing up for the insurance plans, they should be able to say, "Okay, well, with the Medicare Advantage plan, we are getting this quality of cardiac care, this quality of cancer surgical care", and I think that should be an important component. You know, some Medicare Advantage plans may excel in one aspect of care, for example, you know, Alzheimer's care or cardiac care, but may do poorly in cancer surgery care, or cancer care in general. So, I think those are some of the things that the policymakers will need to balance and incentivize.
Medicare Advantage plans are really great at cutting utilization because they manage healthcare effectively, but it does introduce some sort of inefficiencies in the system where everything requires a prior authorization; a lot of physicians are familiar with that - a patient needs life-saving surgery, and the authorization is nowhere to be found for two, three weeks, four weeks, and that's a really difficult problem for the patient to go through, and their caregivers. It's a difficult time for them. So, I think those inefficiencies can be mitigated as long as those who require cancer surgery are seen as a distinct population who need timely access to high-volume surgery. I think modifying MA plans in a better way to reflect that, will be the future.
Dr. Shannon Westin: Yeah. We've seen this come up on the podcast multiple times as we're talking about inequities and quality of care. You know, it's on us as physicians and practitioners to interact with our policymakers. We've not always been really good at that, but I think this type of work that you've done really helps us have that objective data that we can bring to these policymakers so this change can be enacted.
Well, thank you so much, Dr. Raoof. We really appreciate you taking the time being on the podcast.
And again, for our listeners, this was a discussion of “Medicare Advantage: A Disadvantage for Complex Cancer Surgery Patients,” and we were with the first author, Dr. Mustafa Raoof. Please make sure you check it out, and please feel free to check out our other podcasts on the JCO website.
Until next time, this has been Shannon Westin, with JCO After Hours. Have a great day.
The purpose of this podcast is to educate and to inform. This is not a substitute for professional medical care and is not intended for use in the diagnosis or treatment of individual conditions.
Guests on this podcast express their own opinions, experience, and conclusions. Guest statements on the podcast do not express the opinions of ASCO. The mention of any product, service, organization, activity, or therapy, should not be construed as an ASCO endorsement.
Join Podchaser to...
- Rate podcasts and episodes
- Follow podcasts and creators
- Create podcast and episode lists
- & much more
Episode Tags
Claim and edit this page to your liking.
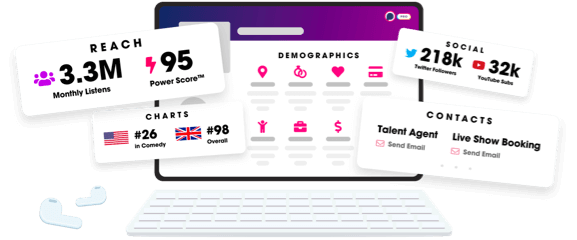
Unlock more with Podchaser Pro
- Audience Insights
- Contact Information
- Demographics
- Charts
- Sponsor History
- and More!
- Account
- Register
- Log In
- Find Friends
- Resources
- Help Center
- Blog
- API
Podchaser is the ultimate destination for podcast data, search, and discovery. Learn More
- © 2024 Podchaser, Inc.
- Privacy Policy
- Terms of Service
- Contact Us
