Growing up in the shadow of Cape Kennedy, Adin Burroughs had designs on becoming an astronaut. But When Adin’s body started rejecting any food he ate with cramps, fever, vomiting, diarrhea - he of course went to his doctor. In Adin’s family, a lot of people have problems with their gall bladder, and Adin told this to his doctor. The doctor ran some tests and declared Adin’s gall bladder as well functioning.
But for the next few years Adin was not able to consume solid food and he lived on soup - all the while seeing numerous specialists in an effort to determine why his body was rejecting the foods he ate.
During the worst periods, Adin would have 27 hours of cyclical vomiting in which he wished for the sweet release of death. As if this wasn’t bad enough, Adin also has the neurological disease of MEcfs and it keeps him bedridden half the time.
In this interview, Adin and I also talk about the relationship between COVID and MEcfs, and how the pandemic may be the best thing to ever happen to MEcfs research funding, care and support.
SHOW NOTES:
0:04:30Adin was born in Orlando, Florida - his parents were rock music promoters - but his parents divorced a couple of years after Adin was born - his mother remarried, and his step father is a college professor of psychology0:05:30Adin was entralled with the nearby by rocket launches and had aims to be an astronaut - but his health came crasing down in 2003 - he had 3 jobs and was on Reserve Duty in New Mexico, and flying to the East Coast to write distributed simulations0:06:30Adin went to the UK to present to the United Nations and then flew home, staying awake for 72 hours - when he got home, his wife was volunteering and he went to help her all day, still no sleep - was awake for 96 hours - and picked up a flu bug with others in his social circle, and half got CFS0:07:30Adin never recovered, he had myalgic encephalomyelitis / chronic fatigue syndrome (ME/cfs) - Adin was admitted to the hospital with 105 degree temperature - they gave him chilled IVs - Adin's job was like an air traffic controller0:08:30About half the people who got the flu with Adin, did not recover, a well defined cluster for studying - but Adin's doctor just shrugged when Adin didn't recover - after initially getting sick, Adin mostly recovered and went back to work - but his temperature flipping around - in the Air Force office they took a thermometer and could see his temperature cycle from 96 to 102 in about 10 minutes - they sent him home0:09:30Adin's wife had to come with him to meet the top brass and help explain what was going on as Adin had developed aphasia (inability to recall words / speak)0:10:30They discovered that Adin's body couldn't control its temperature over 75 degrees, so he had to stay in an air conditioned bubble - his wife quit her job at the University of New Mexico to shuttle Adin to doctors - they thought he had cancer, but couldn't find it - Adin suffered with tachycardia and low blood oxygen saturation, same problem Covid patients are having0:11:30Adin saw many specialists - Adin takes a medication to slow down his heart rate - he takes more than people with heart failure - it took about a hear to see the 6 or 7 specialists - Adin's mom was diagnsoed with MEcfs in 1992, so he knew what the symptoms looked like0:12:30When Adin's body temperature was so erratice, he thought he may have MEcfs, but hoped it wasn't - Dr Nancy Klimas helped Adin's mom, and then Adin0:13:30Adin's wife started to show ME symptoms in 2009, after the birth of their son - she had mild symptoms as first, but in the last year she's gotten sicker - Adin is bed bound about half the time, his wife is bed bound about a 1/4 of the time - she's still in the 'push - crash' phase of exerting too much and then getting sicker and unconscious for 8 - 10 hours0:14:30About 1.5 years ago, their 10 year old son started to show ME symptoms - its hard for a kid: he goes to the playground, but then literally falls over when he gets home and sleeps until morning0:15:30It is hard for adults with ME to learn to not over exert so they don't get sicker, but kids are supposed to be running around - Adin has his son use a Virtual Reality (VR) machine for tai chi, meditation, etc0:16:30Adin also had another medical error: in late 2000s, the ME caused him severe gut problems, he couldn't eat solid food for about a year - Adin was retired from all 3 jobs, but his employers fought over paying Adin, and it was 3 years without pay0:17:30So they lost their house, they lost everything - they had some volunteer lawyers help - during this time, it didn't matter what Adin ate, he'd get stomach cramps, a fever, then vomiting and diarrhea0:18:30Many of Adin's family has gall bladder issues, and tells his doctor this - Adin does a 'fat challenge' (eat a high fat meal) but it had no effect - after 1-2 years, Adin finally got a referral to a specialist at a hospital0:19:30They did a simple sonogram of his abdomen including his liver, stomach and gall bladder - they said Adin's gall bladder was normal - so Adin's GP started barium enemas for lower GI testing - Adin said its some of the worse testing he's been through0:20:30It was painful because they filled his GI tract and put it under pressure to see how it would react - the tech performing the procedure complained the entire time that he was working0:21:30Adin had a lot of testing - endoscopies, colonoscopies, biopsies, food challenges - but the symptoms were only coming intermittently, and then it would be a 27 hour cycle where he literally wished for death0:22:30Adin was in the military, he's been in PoW camps, he knows what pain is like - Adin has a friend who has HIV, and she says it is nothing compared to the horror of ME - but Adin's attacks were lasting 27 hours, the best the doctors could do was give him some meds to control the vomiting and nausea0:23:30But Adin needed to take them at double or triple the max dose - Adin was experiencing cyclical vomiting, kicked off by the gall bladder attack, in conjuction with the autonomic dysfunction caused by ME0:24:30The high doses of those meds were just enough to stop Adin from killing himself to escape the pain and suffering - Adin had said to his wife that he couldn't live that way - the attacks would sometimes also induce tachycardia0:25:30Adin had to go to the ER a few times, but they didn't know how to treat him, his heart, his vomiting - they were scared they were going to lose him - finally, Adin's doctor suggested Adin see a Mayo specialist in cyclical vomiting syndrome0:26:30Adin's evaluation at The Mayo was unlike anything in the regular medial system - he saw 5 specialists a day for a week0:27:30Mayo said that Adin's gall bladder is sludge - it is fine sometimes, but other times fills with sludge - it was easy to see on a common test0:28:30If Adin's doctor had of done the test, it would have cut 2 years of living hell out of Adin's life - Mayo also suggested that Adin's underlying autonomic dysfunction should be looked into, and they had him meet another Mayo specialist - but Mayo would never say anything about Adin's ME, even though he'd been diagnosed by leading doctors and had objective results0:29:30Instead, Mayo would only refer to it as autonomic neuropathy, either central or peripheral - or they would break it down and call it 'post viral fatigue syndrome' - Adin was able to gather from speaking to the staff off the record, that the Mayo had a policy they wouldn't see a patient who had MEcfs0:30:30Adin thinks Mayo had the anti-ME policy because they didn't understand it, they didn't have a black and white test for it, and the expense - most people with MEcfs are unable to work0:31:30A doctor from the VA (Veterans Affairs) wouldn't permit Adin to have a cardiology test because he refused to do an exercise stress test (exercise is contraindicated for ME) - a psychologist told Adin that he was medicalizing psychological issues0:32:30Adin would ask the doctors straight up: 'do you think I'm depressed?' - he wanted them to look him in the eye - they'd say 'no, not depressed' - Adin would ask if it could be MEcfs, and they'd say 'yes', but didn't do anything about it - patients with ME are marginalized, psychologized and traumatized - they are refused services, ridiculed, accused of lying0:33:30Most doctors get stuck on looking for a horse, when ME is a zebra - another analogy is 5 blind men feeling an elephant, none of them has the big picture0:34:30Adin hopes that an outcome of Covid is a systems engineer approach, to take a look at the whole body - it seems self evident medicine should already be doing it0:35:30Covid may be the best thing to happen to ME research - Covid is a systemic infection, and a sign it is like ME0:36:30Unfortunately, there are going to be a lot of Covid survivors who will understand what ME patients have been going through - at least now doctors are realizing that an infection can impact multiple systems - doctors just couldn't wrap their heads around that - they think polio was a one off0:37:30ME was initially called atypical polio - in spite of many medical discoveries, our knowledge of the human body is embryonic - they are just discovering how metabolites impact human health0:38:30Scott says HIV is a walk in the park, but with ME he can't even walk in the park - for Adin, his friend with both HIV and ME saying that living with ME was multiple times harder0:39:30She had experienced multiple trauma, but none of it was from HIV, and she was around in the 80s - she was traumatized by how the medical system treated her ME0:40:30Scott says that 99% of people with HIV and access to meds, are healthier than 99% of people living with ME - it was surprising for Adin to learn that living with ME was so much worse than living with ME0:41:30For the last few years on May 12th, ME patients globally have used their empty shoes as a symbol of the 'millions missing' from life, work, play due to ME - now COVID patients who have not recovered are also displaying their shoes0:42:30Scott says what would also help ME research, is if celebrities and politicians got COVID and did not recover, but develop ME - some celebrities have ME, but they hide it - Cher considers herself recovered0:43:30Celebrities have done the exact opposite of what they needed to do - a famous soccer player got ME, but didn't want to help the community - when Adin was volunteering with Pheonix Rising (a forum for ME patients / caregivers), he met a number of writers who did not disclose their illness because it would impact their career0:44:30The exception is Seabiscuit author Laura HIllebrand - but most don't 'come out' to let the public know that ME is not rare0:45:30There are parallels between ME and HIV in regards to internalized shame - in the early days of AIDS, the slogan was "Silence = Death" - but with ME, there is no high body count, it makes people more susceptible to death by other illnesses - there has only been one case of a death listed as due to ME0:46:30If Adin's mom was to die today, ME wouldn't even be mentioned on her death certificate - the medical marginalization of ME is deeply buried in institutions - for Adin and his family, the quarantine has had no impact - it is the rest of the world that is adjusting0:47:30But they don't have the nausea, pain and suffering that people living with ME have - humans react very differently when things happen to them personally0:48:30Adin deeply hopes that COVID patients recover and that we learn a lot more about how viruses interact with the genome, metabolome, mitochondria - we'll see if the opportunity is squandered or not0:49:30Scott wonders if his HIV meds is why he's healthier than most people with ME - a doctor said that people with HIV and meds who got COVID were not getting as sick as people without HIV (and HIV meds)0:50:30Adin is hopeful for remdesivir for COVID - and that the FDA will do its jobConnect with Adin: https://facebook.com/adindbhttps://twitter.com/adin
Be a podcast patron
Support Medical Error Interviews on Patreon by becoming a Patron for $2 / month for audio versions.
Premium Patrons get access to video versions of podcasts for $5 / month.
Be my Guest
I am always looking for guests to share their medical error experiences so we help bring awareness and make patients safer.
If you are a survivor, a victim’s surviving family member, a health care worker, advocate, researcher or policy maker and you would like to share your experiences, please send me an email with a brief description: [email protected]
Need a Counsellor?
Like me, many of my clients at Remedies Counseling have experienced the often devastating effects of medical error.
If you need a counsellor for your experience with medical error, or living with a chronic illness(es), I offer online video counseling appointments.
**For my health and life balance, I limit my number of counseling clients.**
Email me to learn more or book an appointment: [email protected]
Scott Simpson:
Counsellor + Patient Advocate + (former) Triathlete
I am a counsellor, patient advocate, and - before I became sick and disabled - a passionate triathlete. Work hard. Train hard. Rest hard.
I have been living with HIV since 1998. I was the first person living with HIV to compete at the triathlon world championships.
Thanks to research and access to medications, HIV is not a problem in my life.
I have been living with ME (myalgic encephalomyelitis) since 2012, and thanks in part to medical error, it is a big problem in my life.
Counseling / Research
I first became aware of the ubiquitousness of medical error during a decade of community based research working with the HIV Prevention Lab at Ryerson University, where I co-authored two research papers on a counseling intervention for people living with HIV, here and here.
Patient participants would often report varying degrees of medical neglect, error and harms as part of their counseling sessions.
Patient Advocacy
I am co-founder of the ME patient advocacy non-profit Millions Missing Canada, and on the Executive Committee of the Interdisciplinary Canadian Collaborative Myalgic Encephalomyelitis Research Network.
I am also a patient advisor for Health Quality Ontario’s Patient and Family Advisory Council, and member of Patients for Patient Safety Canada.
Medical Error Interviews podcast and vidcast emerged to give voice to victims, witnesses and participants in this hidden epidemic so we can create change toward a safer health care system.
My golden retriever Gladys is a constant source of love and joy. I hope to be well enough again one day to race triathlons again. Or even shovel the snow off the sidewalk.
From The Podcast
Medical Error Interviews
Interviews with survivors, victims' families, policy makers, and health care workers. What went wrong? How can we make health care safer? Host Scott Simpson, uses his counselling skills to evoke the secrets, stories and solutions. Be a Patron at Patreon.com/MedicalErrorInterviewsJoin Podchaser to...
- Rate podcasts and episodes
- Follow podcasts and creators
- Create podcast and episode lists
- & much more
Episode Tags
Claim and edit this page to your liking.
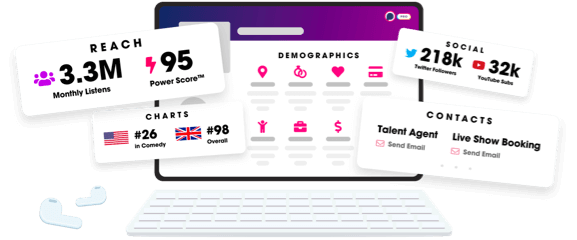
Unlock more with Podchaser Pro
- Audience Insights
- Contact Information
- Demographics
- Charts
- Sponsor History
- and More!
- Account
- Register
- Log In
- Find Friends
- Resources
- Help Center
- Blog
- API
Podchaser is the ultimate destination for podcast data, search, and discovery. Learn More
- © 2024 Podchaser, Inc.
- Privacy Policy
- Terms of Service
- Contact Us
