Dr. Charles Raison is an American psychiatrist and professor of psychiatry at the University of Wisconsin-Madison School of Medicine and Public Health as well as the Mary Sue and Mike Shannon Chair for Healthy Minds, Children & Families and Professor with the School of Human Ecology in Madison, Wisconsin.
Show More
Suggest an edit
Followers
1
Creator Details
Birthdate
Dec 26th, 1957
Location
Atlanta, Georgia, United States of America
Episode Count
3
Podcast Count
3
Total Airtime
2h, 3m
PCID
Suggest an edit
Manage This Profile
Are you Dr.? Verify and edit this page to your liking.
Dr. Charles Raison's Creator Profile
This is a podcast creator profile for Dr. Charles Raison. This page showcases all of Dr. Charles Raison's podcast credits and appearances such as hosted episodes, guest interviews, and behind-the-scenes work. You can follow this profile to get notifications of Dr. Charles Raison's new podcast credits.
Join Podchaser to...
- Rate podcasts and episodes
- Follow podcasts and creators
- Create podcast and episode lists
- & much more
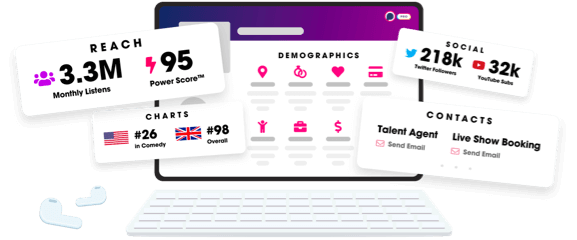
Unlock more with Podchaser Pro
- Audience Insights
- Contact Information
- Demographics
- Charts
- Sponsor History
- and More!
- Account
- Register
- Log In
- Find Friends
- Resources
- Help Center
- Blog
- API
Podchaser is the ultimate destination for podcast data, search, and discovery. Learn More
- © 2024 Podchaser, Inc.
- Privacy Policy
- Terms of Service
- Contact Us