Dr. Karen Wyatt founded the End-of-Life University. Hear how her father's suicide lead her to learn about hospice and a career that focuses on helping educate people about end-of-life care. Contact End of Life University Note: A Life and Death Conversation is produced for the ear. The optimal experience will come from listening to it. We provide the transcript as a way to easily navigate to a particular section and for those who would like to follow along using the text. We strongly encourage you to listen to the audio which allows you to hear the full emotional impact of the show. A combination of speech recognition software and human transcribers generates transcripts which may contain errors. The corresponding audio should be checked before quoting in print. Transcript Dr. Bob: On this episode, I'm speaking with Dr. Karen Wyatt. Dr. Wyatt is a family practice physician who specialized in hospice medicine for many years, and more recently has created the End of Life University, which is an online site that provides education and tools for people to learn about and become more comfortable with approaching end of life and having the most peaceful and dignified end of life possible. She's also an author, has written several books, including What Really Matters, Seven Lessons for Living From the Stories of the Dying. She also wrote a book called the Tao of Death and A Matter of Life and Death. She is a speaker and a great advocate for excellent, compassionate end of life care. During our interview, there were a couple of little connectivity issues, so there's a couple of very brief glitches. I hope it doesn't take away from the valuable content. You'll get some phenomenal insight and inspiration from this interview. Thanks for tuning in. Thank you, Karen, for being on our show today. Dr. Karen Wyatt: Hi, Bob. Thank you so much for having me. Dr. Bob: We had a chance to talk a couple of weeks age when I was interviewed for your podcast, and it was a great conversation. I think we both recognize that we have so much alignment, so many things in common regarding our careers and kind of where our priorities are, where our visions are trying to take us. You probably see this as well. Most of the people who are really passionate about providing great care for people at end of life have a personal experience or a personal story that kind of fuels their drive and their passion for that. I know you have one as well. Can you share a bit about how you became so aware of the importance of providing really phenomenal end of life care and making appropriate preparations? What's your story? Dr. Karen Wyatt: Yes. I'm happy to share that, Bob. It started for me a long time ago, when I was just a young doctor, brand new in medical practice, and I had trained in family medicine, but honestly had no training whatsoever in end of life issues. I hadn't received any ... at all around death and dying, which is shocking really when I look back and think about that. I really didn't have any knowledge or awareness of end of life issues and what was happening in that arena. But at that time I was in my early 30s, and my own father committed suicide, which was a horrific tragedy for me and my entire ... , but particularly devastating to me, because I was a doctor, because I had done extra training in psychiatry, just so that I could treat people with depression, and I had worked with some suicidal patients in my practice. The fact that I couldn't help my own father just completely tore me apart and really caused me to question, "Am I even a good doctor? Should I even be doing medicine?" I floundered for about three years with just overwhelming guilt and grief after my dad's death. One day I got the idea to call hospice, even though at that time I wasn't even really sure what hospice did. I knew so little about it, but this inspiration just popped into my head, "Call hospice." I called and had a chat with them, the hospice in my community, to see if I could volunteer in any way. It turns out their medical director had just resigned 30 minutes before I called, and so she said, "Actually, we have a job for you right now." Knowing almost nothing about hospice, or death and dying, or end of life care, I became a hospice medical director. From that moment on, my training started in really learning about dying. I was trained by the nurses. Our hospice at that time had nurses who had worked there for 10 and 15 years, caring for dying patients. I just followed them everywhere. I sat with them, and I just soaked up all this wisdom, and experience, and knowledge from them, all things that, looking back, I know I should have learned as a doctor. It was embarrassing that, as a doctor, I knew so little, but once I started making home visits to patients in hospice, I realized this is where I'm meant to be. This is the kind of medicine I was meant to do all along. It felt like I was home in a way like I'm doing what I'm supposed to be doing now. It was a huge relief to me professionally to be finally offering the kind of care I wanted to give. I loved the fact that hospice was team-oriented, so I got to work with other people, with nurses, and home health aides, and the social work, and the chaplain, and we would all meet together to provide care as a team. That really fit perfectly with how I thought care should be offered to all patients, not just end of life patients. I spent many years doing hospice full time. I left family practice, did only hospice for a number of years. I just had profound experiences there, and I can say really by just immersing myself in death and dying is the way I found my way through that horrible grief and guilt that I was carrying after my dad's death. Long story, but as it goes, I ended up deciding I wanted to write a book about patients I had cared for. ... It took me many, many years to actually do that, find the time and get the book written, but I finally got that done, and I ended up leaving medicine in order to start writing. That happened eight years ago. Now I haven't been in clinical practice. I've been doing more writing, and speaking, and educating for the past eight years. Dr. Bob: Do you feel like the time you have devoted to A, caring for patients and being a part of that amazing hospice team and the work that you've done as a teacher and a writer, have you eased your conscience? Have you gotten to a place where you're not feeling guilty about what happened at this point? How has that worked? Dr. Karen Wyatt: Yeah. I would say it's much better now ... what I've begun to see over time, and it took a lot of years, is my dad was on his own path. He made his own choice and that really I couldn't have interrupted it. It was his decision, and he was determined to do what he did, and that my life intersected with my dad's life, because I was on my path, and his death is really what shifted me I think to a place I needed to be and a place I needed to go, and that without his death, I probably would never have ended up in hospice, and not that I'm saying that's a justification or the reason why my dad died, but it all fit together in that way and kind of brought me to a place where I needed to be. So, I was able to let go of feeling responsible for my dad, and allow my dad the responsibility for his own choices, and feel like I at least was able to make something beautiful out of the tragedy that happened. Dr. Bob: That experience, it's interesting, because I talk to so many people who go through a death, they go through what's a tragic loss, and ultimately there's something powerful and amazing that comes out of that. I couldn't say that that's ubiquitous, and it happens in every case, but I know a number of people, and myself included, where death has resulted in a transformation of some sort that clearly would not have taken place without the death having occurred. I think about the silver lining of life and death. For myself, the first real, peaceful death that I ever encountered or was part of that experience was my friend, Darren Farwell, who died at 32 back in 2001, and for me that was what planted the seed of wanting to provide this amazing type of care to people, you know, this interdisciplinary, holistic, compassionate type of care, because I got exposed to hospice for the first time. Then additionally, his wife ended up creating a foundation to help ... He died of melanoma, and his wife, Rhonda, created a foundation to help support education about the dangers of the sun and then built a company called UV Skinz that makes UV protective clothing and swimwear, which has grown into a phenomenal company. I see these UV Skinz being worn all over the beaches of San Diego and Hawaii. I talked to so many people over time who have been able to make something remarkable happen as a result of having experienced a death in their life. I'm assuming that you've had similar experiences. Dr. Karen Wyatt: Oh, yes. So many times, through the interviews that I do as well for End of Life University and just people that I've met, in this grief work really, that sometimes as our way of working through grief we take up a project or make a change in our lives. It can be profound, but all of these people, as you're describing, talk the same way, that it was a transformation for them. They really feel like they became the person they were meant to be, who they were meant to be, true path, true calling, once they worked through the grief that they experienced from tragedy. Dr. Bob: Interesting. It's not necessarily the death, the loss, the change that occurs because of that. It's the work that goes into the grief process and sort of the rebuilding of a life after the loss. I'm sure it's all part of it, right? Dr. Karen Wyatt: Yeah. Dr. Bob: But I guess that's probably an important component of it, the work that goes in, and what we learn about ourselves, and the other support that we may get that guides us after that experience. Dr. Karen Wyatt: Yeah. So true. It all fits together, but I think death really awakens us and helps us learn to cherish life and then make the most of it too when it hits us that wait a minute. I won't be here forever. This is limited. I need to make sure that I make the most of every moment that I have. Dr. Bob: I mean, wouldn't it be nice if somebody could have that awareness and gain that awareness without having to go through that experience? I guess maybe that's partly what we're trying to do, right? Dr. Karen Wyatt: Yeah. I've wondered about that, like is it really possible for someone to grasp that? But yes. I think most of the information I disseminate has that purpose behind it, that if only someone hears this, will learn something, will open their eyes a little bit and recognize that natural part of life for everyone, so they need to pay attention to it and be aware of it. Dr. Bob: Yeah. Well, the work that you're doing now, you're very prolific. You're putting out a lot on your website, and you're creating groups. I know you created The Year of Reading Dangerously, a book club to help people get exposed to books that are out there that could give them a new perspective and bring more value. Can you share a little bit about what you've experienced through creating that one program? I know there are others, but I wanted to kind of focus a little bit on that one. Dr. Karen Wyatt: Yes. Well, it's interesting. I got the idea at the end of last year. It would be really cool to do an online reading group or book club, because I had written a blog post about how to start an end of life book club in your community, and I heard back from several people that because of that blog post, they had done a year-long book group, reading books about death and dying. I thought, "But what if I could do it online and have a bigger group [inaudible 00:14:15]?" I had no idea if it would resonate with people if anyone would even be interested and would sign up. I just posted it right around New Year's Day. I posted a little message on Facebook, you know, for my Facebook followers and said, "I'm starting this reading group. You can sign up here if you're interested." That was right before I went to bed one night, and I woke up in the morning, and ... already ... reading group, and within a week I think I had 600 people on the list. That post about the reading group had been shared 57 times, so people were sharing it with other people they knew. Now we have 830 people who signed up for the reading group. We're just reading one book each month during the year of 2018. ... Each month I'm doing a conference call discussion of the book. Most of the authors of the books I've chosen for this year have agreed to come on the call and actually be there for a Q&A session. Dr. Bob: Oh. That's phenomenal. Dr. Karen Wyatt: It's really exciting and really fun. I've been fascinated to see the people who are joining the group. At first, I thought it'll just be all the same people. It'll be all the same people that already do this work who are interested, but I'm getting a lot of people are writing in on the Facebook group, "I know that it's time for me to start looking at death and dying, and I thought this would be a good way to get introduced to it." I'm excited. It was just a fun, little experiment, but it turns out that it does seem to be something people are looking for. Dr. Bob: Well, clearly. I'm part of that group now as well. It seems like there really is a growing sense of desire for people to connect around the topic of death and dying. I started a meetup here in San Diego as well, called Reimagining End of Life Care. The idea is I just want to bring people together from all different walks of life who are interested in talking about, sharing ideas, looking at the issues, trying to bring their own unique perspective and gifts, whether that's a nurse, or a doctor, or a social worker, or an Uber driver, or somebody out in the community. There are 120 people in the first couple of days joined this meetup group, because I think it's just something that's sparking interest. People are getting more comfortable exploring. I think people recognize that if you just allow things to happen by default, there's a good chance that they won't go well. There's more awareness of that. Dr. Karen Wyatt: Yes. Definitely. I think this interest has really grown just in the last three to four years. I don't know if you've experienced that, but it seems like there's momentum now behind it. More and more people are starting to wake up and be at least less afraid of talking about death and dying. They might still be afraid of death itself, but they're less avoidant of the subject now. Dr. Bob: I think that there's growing awareness. There are the death cafes that are popping up. I guess I'm a little bit unsure whether it's just the world that I'm living in, and so I'm much more aware of it, or if it's really happening. I'm going to assume that it's really happening. I'm going to make that decision to choose to believe that it's happening, and we are part of that momentum, and we can help I think, through our experiences and through our desires, try to help to guide people to understand what they can do, what each individual can do to have A, the best possible end of life experience for themselves, to help guide others in their sphere of influence. I think like you clearly believe that the best way to have a good experience or the best chances of having a good experience is to be ready, is to be prepared, is to understand what the potential issues are, what you need to put in place to make sure that you have the best chances of having your end of life go the way that you would want it to go. Dr. Karen Wyatt: Exactly. If you even think about it, would you ever go on a journey to a place you've never been before without preparing for it ahead of time, without reading about it and learning what you need to do in advance before that trip? Getting ready for the end of life, it's really similar. You're just learning as much as you can and preparing yourself, so that you can make choices in the moment when you need to, and that you're ready for whatever might come up on that journey that you're going on. Dr. Bob: You know, I like that analogy. There are people who don't want to plan and are going to take a trip, and they're just going to start driving, right? They may know what their ultimate destination is, or they may not even know what the ultimate destination is, but they're okay with things just kind of happening and rolling with it. There are people who will live their life that way, and not plan, and not prepare, and take their chances. That's okay. That's your choice. The problem though with that is that if that's the way you choose to proceed, somebody may end up taking the flack for that, right? Your loved ones, your family members, somebody's may end up having to make choices that they're not prepared for and have to deal with kind of the fallout, which we see all the time, right? Dr. Karen Wyatt: Yeah. So true. Yes. Exactly. The loved ones might be left with terrible grief, and guilt, and a burden of having to make decisions, and that's something we all need to remember. How do we want our loved ones ...? How do we want to leave them when we do go? Dr. Bob: Sometimes people, they need a little bit more incentive than just doing it for themselves. We all know that it's important to plan and to create advanced healthcare, or we should all know that it's important to have advanced healthcare directed, to have a will, to have these things set up, so that your loved ones won't have to try to figure it out in the heat of things, but I think one way to help to inspire, encourage, incentivize people is make sure that they understand that they'll be gone or they'll be unconscious, but it's the people they care about who are going to potentially carry this burden and potentially carry guilt around with them and regret for the rest of their lives. Do it for them. If you're not going to take care of your documents, and your paperwork, and put things in place for yourself, do it for your children. Do it for your siblings. I think it's a really important message for us to share. Dr. Karen Wyatt: Absolutely. I do know many people who say, "I don't care that much what happens to me, so why should I plan." Your message is perfect, because you do care about what happens to your loved ones, and you want them to have as much peace of mind as possible. Dr. Bob: You've put a lot of things in place, and I really encourage everyone who's listening to go to Karen's website, because there's just a wealth of information, resources, and tools that are out there that can help people move forward with this kind of planning. Can you share a little bit about how that's all kind of come together? Dr. Karen Wyatt: Yes. I started End of Life University actually after I wrote the book, the book I mentioned of stories about hospice patients, and it came out six years ago. I decided I have to do something more than just putting a book out there in the world. That's when I started doing interviews for End of Life University with people who work in all aspects of the end of life arena. I do two interviews every month on End of Life University, and your interview is upcoming in March, the one I did with you. Then I repurpose some of those interviews and have a podcast on iTunes, just like your podcast, that comes out weekly, but I keep getting more and more ideas. I start something good [inaudible 00:23:32] new idea, like, "Oh, wait. That's not enough. I need to do something more." Besides the interviews, I created ... for end of life planning, called The Step-By-Step Roadmap to Planning for the End-of-Life. So, it's just a little course, a self-directed course that walks people through the steps they need to take in order to get their paperwork done, and I'm working on other courses right now, courses to train people to become death educators in their community, to go out and start workshops, to become an educator in their own community for their neighbors and friends. Dr. Bob: So, spreading it out, right? I mean, there's so much need, and there's so much work to be done. Obviously, it's going to take a tribe, a village, and so like me, you're bringing together a tribe of people who want to make sure that the experience at end of life is as dignified and peaceful as possible. It starts so far upstream. When we think about end of life and having a peaceful end of life, you think about those last few days or weeks, but it really is so important to be working with people either before they're diagnosed with a serious illness or at the time of diagnosis. We can't wait until just those last few days of life to put in place the things that are going to allow for a peaceful and dignified transition. Dr. Karen Wyatt: Yes. That's so true. Dr. Bob: We have to have a different conversation about continuing or discontinuing treatments. I'm sure you've experienced this as well. The medical community is so reluctant or unable to dive into those deep conversations with people about the potential impact of some of the treatments or the other options that are available. I hear it all the time from patients, you know, "My doctor would never talk about that. They wouldn't go down that path with me. They only gave me this one option." I just heard from somebody yesterday who was seeing an oncologist for esophageal cancer, and when she told the oncologist that she didn't want to do yet another course of chemotherapy because the tumor was still growing ... She'd had very toxic side effects from it, and she just wanted to try to have the last few months of her life not feeling sick all the time, knowing that at some point the cancer would progress, and she would be very compromised, but she wanted this window of time. Her doctor basically told her not to come back, "There's nothing more that I can do. If you're not going to take my advice and go with my recommendations, then here's a number for hospice," which is so wrong. Dr. Karen Wyatt: Wow. Oh. Absolutely. It's heartbreaking because a patient who's been working with a doctor for sometimes year in treatment and then suddenly the doctor abandons that patient and says, "I don't want to see you again," it's tragic. Now ... doctor, who now is not going to be exposed to the actual end of life process for his patients. He's refusing to even deal with that portion of her life as it plays out, and it's really sad for that doctor, who won't get the advantage of seeing what's possible for a patient. That just breaks my heart. Dr. Bob: It did for mine as well. I hear stories like that not infrequently. In this particular patient, she wanted to access a prescription through medical aid in dying, not that she's ready to end her life, but she knows what the ultimate course of metastatic esophageal cancer is, and it's not pretty, so she wants to be prepared, have that option. She asked her oncologist if he was in support if he could help her or even guide her, and his response was, "I don't do that. Here's a number for hospice," which again, I don't want to label all ... I don't want to generalize, but I do feel that the medical community is doing a disservice to people by not recognizing that this period of time between aggressive treatment and death, it could be so much better supported, and there's so much more that can be done, but they don't understand it. Dr. Karen Wyatt: Yes. I would say one of my goals ultimately is to work with my colleagues in medicine and help [inaudible 00:29:02] and open their eyes to death and dying, but I realize that may not happen until we kind of galvanize their patients. We need to ... . At the grassroots level, we need patients going to their doctors saying, "You have to talk to me about and deal with me about this." I was really thrilled a few weeks ago. I got an email from a woman who had been listening to my podcast, and she and her husband are both in their 70s. She said, "We listened to your podcast about how patients need to bring up the topic with their doctors." She said, "We brought in our ... will, and we sat with our doctor and said, 'We want to go over this with you.'" She said, "His eyes got huge, and he backed toward the door and was saying, 'No. No. No. We don't need to talk about this.'" They insisted, so he sat down with them. He answered their questions. They went through their living wills together. In the end, he seemed grateful. He thanked them and said, "I'm glad that you brought this up." I was so thrilled. It actually does work. If patients will have the courage to insist that their doctors talk with them, I think the doctors will ultimately say, "Okay. I'll look at this with you." Dr. Bob: We might not get every one of them, but I think that's one certain definite strategy. Like you said, that physician was grateful. That very well may have shifted his practice, right? That one encounter, that one experience he might have recognized, "Wow. This is really meaningful, and this is important stuff, and it's not hard." Right? It's not all that difficult. It just takes a little bit of time. Dr. Karen Wyatt: Yeah. If you haven't been introduced to it or trained to have the conversation, it feels much more intimidating, and it is in your mind, than it really is once you start talking about it. I think that becomes an obstacle to physicians to bring up the subject, but once they've done it, they can realize, oh, it actually feels comfortable, and it actually it's kind of a relief, once we get these issues out in the open and discuss it together. Dr. Bob: Well, Karen, I think you and I have a lot of good work to do, both individually and together. I think, as we've been talking about, there are some great opportunities to bring our tribes together, and continue moving the needle in the right direction, and trying to give as many people as possible the tools that they need, the inspiration they need to put in place what they can to ensure that as their life is coming to a close, as they're dealing with these health challenges, that their values and their wishes are honored. I'm really happy to be in partnership with you on that. Dr. Karen Wyatt: Same here. Same here. It's good to join forces. Dr. Bob: Yeah. You got a lot of, as we mentioned, a lot of great material and resources, so how do people tap into that? What's the best way for people to access what you've put together? Dr. Karen Wyatt: They can go to EOLUniversity.com. That's my website, EOL standing for end of life, but EOLUniversity.com. There they can connect to the podcast and blogs I've written. They can learn about upcoming interviews, find my books and courses, so I need to update that a little bit, but they should be able to find everything at EOLUniversity.com. Dr. Bob: Yeah. Well, you've done a phenomenal job. When you go to her website, don't be overwhelmed. There's a lot of information, but just take it a bit at a time. Dive in. If you're interested in, I guess in just dipping your toes in the water of this, then maybe sign up for the Year of Reading Dangerously Book Club and start with one or two of those books. We will, I'm sure, have more time, opportunities to connect and collaborate. Again, I appreciate you taking the time. I love our conversations because it's just sort of like talking to myself, but with somebody smarter. Dr. Karen Wyatt: Yeah. It's wonderful. It's wonderful for me too, Bob, to be speaking to somebody like-minded, so thanks so much for this opportunity. Dr. Bob: Yeah. Thank you for taking the time. Thank you, listeners, for tuning in. Until next time, have a wonderful day, and give your loved ones a big hug and a kiss. Take care.
From The Podcast
A Life & Death Conversation with Dr. Bob Uslander
In this podcast, we talk about life, death and everything in between. We'll explore how to age more gracefully, have meaningful conversations, and what you can do now to ensure the best possible end-of-life experience for yourself and your loved ones. Let's get friendlier with death.Join Podchaser to...
- Rate podcasts and episodes
- Follow podcasts and creators
- Create podcast and episode lists
- & much more
Episode Tags
Claim and edit this page to your liking.
Unlock more with Podchaser Pro
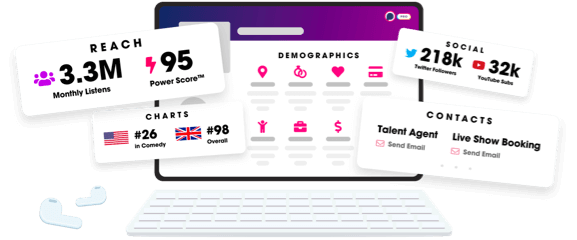
- Audience Insights
- Contact Information
- Demographics
- Charts
- Sponsor History
- and More!
- Account
- Register
- Log In
- Find Friends
- Resources
- Help Center
- Blog
- API
Podchaser is the ultimate destination for podcast data, search, and discovery. Learn More
- © 2024 Podchaser, Inc.
- Privacy Policy
- Terms of Service
- Contact Us
