Coordination of Benefits (COB) is a term used by healthcare organizations which explains the determination of benefits for a patient with multiple insurance plans. There are many rules and regulations made by The American Dental Association (ADA) to accurately coordinate patient’s benefits. Following these rules will help avoid delays in payment and will ensure that insurance companies process claims correctly!How does a patient end up with multiple insurance plans? Many different ways, but there are a few common examples to remember. It is common to see a child with dual coverage because both parents have their own insurance coverage. Of course, the child would have to be enrolled in both parents’ plans. Using the same scenario, can we assume that both parents also have dual coverage? If both insurance plans cover families/spouses, then it is definitely safe to assume. A few other reasons a patient might have dual insurance:Being a part of a federal insurance plan (Ex. FEHB and FEP)Being qualified for MedicaidBeing an adult child (under 26) who has his or her own coverage and also through their parentsPatients may be thinking, “I have two insurance plans; so that means I would get double the benefits?” That is not always the case. Having two or more insurance plans does help cover insurance expenses better through the coordination of benefits provisions. Giving your patient knowledge about their dual insurance benefits before treatment is essential. Yet again another reason insurance verification is so important. So how can we determine the order of benefits for patients with dual insurance? There are many rules to remember when setting up a patient’s account. Here are the most common rules used to determine benefits:Birthday Rule - Child has coverage from both parents' insurance plans. The parent whose birthday falls earlier in the calendar year is primary. If the parents have the same date of birth it is determined by who has had coverage the longest with the insurance company.Subscriber Rule - When the patient is the subscriber, employee, member, policyholder of the insurance plan he or she is always primary on that plan. Any other plans where the patient is a dependent would be their secondary plan.Medicare Rule - Medicare is secondary to the plan covering the patient as a dependent.Divorce Rules - If a court decree states one of the parents is responsible for the child’s health care expenses/care, the plan of that parent is primary. No court decree? - Order of benefits are as follows:The plan covering the custodial parentThe plan covering the spouse of the custodial parentThe plan covering the non-custodial parentThe plan covering the spouse of the non-custodial parentDental offices need to have a basic understanding of these rules to properly handle account setups. The dental office is also responsible for making sure their patients properly understand their benefits, especially when dealing with dual insurance. This conversation should happen with the patient during treatment plan negotiations. Before all of this happens, your office must verify patients’ benefits through your insurance verification process.
From The Podcast
Dental Billing Support Podcast
This Podcast is geared towards anyone working in the dental industry, whether they are Dentists, Office Managers, Insurance Coordinators, Dental Billers, etc. It will help a lending hand to anyone that has a question or questions regarding insurance posting, adjustments, primary/secondary/tertiary claims, claim submissions, xrays, insurance aging reports, insurance specific questions, etc. It can also be software based questions, OpenDental, Dentrix, Eaglesoft, Curve, Practiceworks, SoftDent, etc. For questions or to follow along, please join our Facebook Group: Dental Billing Support GroupAbout the Hosts: Davy Clay, MBA, CDCDavy Clay is an Expert Dental Billing Consultant with 10+ Years experience working in the dental billing and dental insurance industry. His passion is helping dentists and their staff to realize and change the inefficient, inexperienced, and sometimes illegal billing practices taking place within dental practices. With an Insurance degree from University of Georgia and MBA from Georgia Southern University, Davy started Dental ClaimSupport in 2012 after working for Howard Family Dental as the Head of the Billing Department running the billing for their eight practices.Josh Smith, CDCJosh Smith is a co-founding partner of Dental ClaimSupport. Originally from both Augusta, GA and Savannah, GA, Josh attended the University of Georgia and graduated with a Real Estate Degree from UGA’s Terry College of Business. Upon graduation, Josh moved to Beaufort, SC to pursue his career in the dental field as both an Office Manager and Billing Coordinator as well as receiving his CDC certificate.Join Podchaser to...
- Rate podcasts and episodes
- Follow podcasts and creators
- Create podcast and episode lists
- & much more
Episode Tags
Claim and edit this page to your liking.
Unlock more with Podchaser Pro
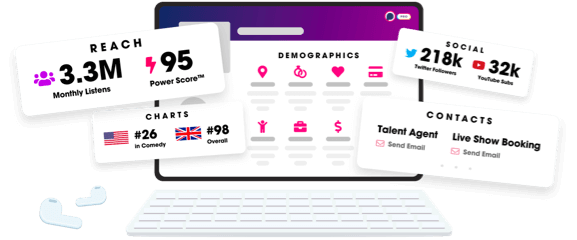
- Audience Insights
- Contact Information
- Demographics
- Charts
- Sponsor History
- and More!
- Account
- Register
- Log In
- Find Friends
- Resources
- Help Center
- Blog
- API
Podchaser is the ultimate destination for podcast data, search, and discovery. Learn More
- © 2024 Podchaser, Inc.
- Privacy Policy
- Terms of Service
- Contact Us
