While COBRA has fairly straight forward effects, the qualifications and details are quite nuanced. Joining the show to help small business owners stay compliant with COBRA is Operations Manager, Benefits at Asure, Heather James!
Heather joins Mike Vannoy to dive into the history and regulations of COBRA. Heather explains the different qualifying events, the regulations for notifying an employee, and who COBRA applies to.
Takeaways:
- While many people think COBRA is insurance, in reality it is a law that requires employees still have access to group plans when they go through a qualifying event like leaving the company.
- COBRA requires that the employee must pay for the remaining benefits in full. The employee must pay both their previous contribution, and the previous employer's contribution. In some cases there is also a 2% administration fee.
- The DOL has strict regulations about notifying an employee about their COBRA eligibility, even down to font size and bolding. When notifying an employee, make sure you comply with the rules and regulations.
- As an employee, when you receive your packet from your employer, you have 60 days to make a decision as to your course of action. COBRA doesn’t kick in until your decision, but is applied retroactively to the date you lost your active policy.
- While many people think COBRA only applies to terminations, there are a few other qualifying events. Moving from full time to part time qualifies you as you are losing access to your healthcare benefits despite still working at the company.
- COBRA applies beyond just the employee and to their dependents. A divorced spouse or a dependent who turns 26 and ages out of coverage are both types of qualifying events for COBRA.
- A common mistake employers make is not notifying their employees properly and through the correct channels. Every qualifying event needs to be notified for, and all notifications must happen through the US mail.
Quote of the Show:
- “COBRA is not the actual insurance, COBRA is the continuation of those rich group plans that you had.” - Heather James
Links:
- LinkedIn: https://www.linkedin.com/in/heather-james-4a727b16/
- Company Website: https://www.asuresoftware.com/
- DOL Website: https://www.dol.gov/agencies/ebsa/laws-and-regulations/laws/cobra#employers
Ways to Tune In:
- Spotify: https://open.spotify.com/show/2XThTdn7YC1lkAm0PgZUkj
- Apple Podcasts: https://podcasts.apple.com/us/podcast/mission-to-grow-a-small-business-guide-to-cash-compliance-and-the-war-for-talent/id1725890976
- Amazon Music: https://music.amazon.com/podcasts/328dddd0-3c4f-4b07-a0d3-13bdcb418486/mission-to-grow-a-small-business-guide-to-cash-compliance-and-the-war-for-talent?refMarker=null
- Audible: https://www.audible.com/pd/Mission-to-Grow-A-Small-Business-Guide-to-Cash-Compliance-and-the-War-for-Talent-Podcast/B0CS71KQFM?qid=1706208857&sr=1-1&ref_pageloadid=not_applicable&ref=a_search_c3_lProduct_1_1&pf_rd_p=83218cca-c308-412f-bfcf-90198b687a2f&pf_rd_r=A1ME8MBECSVZ6K4D7CNT&pageLoadId=QBtg12mqKsuZPLGY&creativeId=0d6f6720-f41c-457e-a42b-8c8dceb62f2c
- Podchaser: https://www.podchaser.com/podcasts/mission-to-grow-a-small-busine-5591006
Show More
Rate
From The Podcast
Mission to Grow: A Small Business Guide to Cash, Compliance, and the War for Talent
Welcome to Mission to Grow, the podcast tailored for small business owners seeking practical insights, compliance-oriented content, and expert advice to navigate the complexities of HR and beyond. Hosted by Mike Vannoy, a seasoned business professional with a vision for rebranding and leveling up. Join us every Thursday as we delve into the world of compliance, productivity, and management strategies to empower owners and managers of midsize companies.Join Podchaser to...
- Rate podcasts and episodes
- Follow podcasts and creators
- Create podcast and episode lists
- & much more
Episode Tags
Do you host or manage this podcast?
Claim and edit this page to your liking.
,Claim and edit this page to your liking.
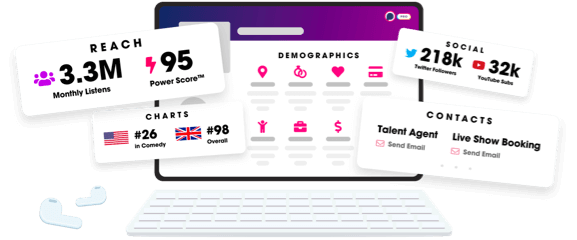
Unlock more with Podchaser Pro
- Audience Insights
- Contact Information
- Demographics
- Charts
- Sponsor History
- and More!
- Account
- Register
- Log In
- Find Friends
- Resources
- Help Center
- Blog
- API
Podchaser is the ultimate destination for podcast data, search, and discovery. Learn More
- © 2024 Podchaser, Inc.
- Privacy Policy
- Terms of Service
- Contact Us
