Episode 170: Schizophrenia: An Overview
Future Dr. Chng explains the diagnostic criteria and describes how to treat schizophrenia. Dr. Arreaza mentions additional risk factors and social aspects of schizophrenia.
Written by Tiffanny Chng, MSIV, Ross University School of Medicine. Comments by Hector Arreaza, MD.
You are listening to Rio Bravo qWeek Podcast, your weekly dose of knowledge brought to you by the Rio Bravo Family Medicine Residency Program from Bakersfield, California, a UCLA-affiliated program sponsored by Clinica Sierra Vista, Let Us Be Your Healthcare Home. This podcast was created for educational purposes only. Visit your primary care provider for additional medical advice.
Schizophrenia may be an intriguing disease for many, even for health care providers. Schizophrenia is frequently misunderstood and stigmatized. Receiving a diagnosis of schizophrenia can be life-altering and cause significant distress in patients and their families, but it can also impact their work, relationships, and even their communities.
Epidemiology of schizophrenia:
Schizophrenia has a prevalence of about 1% worldwide, and a prevalence of about 0.6% in the US. Although the distribution between males and females is comparable, males will typically present with their first episode, sometimes known as a “psychotic break” in the early 20’s as opposed to women who may present in their late 20s or early 30s. Despite having a low prevalence, the NIH lists schizophrenia as one of the top 15 leading causes of disability and disease burden in the world.
In 2019 the economic burden of schizophrenia in the US was $343 billion. For comparison, in 2019, diabetes had an economic burden of $760 billion in the US, however, the prevalence of diabetes that year was 11.6%, more than 10 times that of schizophrenia.
Patients who are diagnosed with schizophrenia are also at increased risk of a multitude of co-occurring medical conditions: alcohol and substance abuse disorders, mood disorders, and metabolic disturbances (diabetes, hyperlipidemia, and obesity, which may be exacerbated with the use of antipsychotics). These patients have a two-to-four-fold increased risk of premature mortality with an estimated potential life loss of ~28.5 years. Of note, 4-10% of patients with schizophrenia die secondary to suicide.
Pathogenesis:
The exact pathogenesis of schizophrenia is unknown, but we do know that it is a combination of genetic, neurological, and environmental factors.
Genetics: Twin studies conducted in mono and dizygotic twins have shown that schizophrenia is highly inheritable (~80%). Although there are no specific genes that directly cause the disease state, genome-wide association studies have shown polygenic additive effects of 108 single nucleotide polymorphisms. This includes genes involved in the dopaminergic and glutamate pathways, which are the basis of antipsychotic medications.
Epigenetics: Studies have also shown that epigenetics is a potential factor that plays into the risk of developing schizophrenia. Having a history of obstetric complications, for example, has an almost two-fold increased risk of schizophrenia in the child during early adulthood. Such complications include maternal infections, preterm labor, and fetal hypoxia. Certain infections and pro-inflammatory disease states, such as Celiac and Graves’ disease have also been associated with schizophrenia. The suggested pathophysiology is thought to involve pro-inflammatory cytokines crossing the blood-brain barrier inducing or exacerbating psychosis or cognitive impairment.
Trauma: As in many other psychiatric conditions, childhood trauma or severe childhood adversities, especially emotional neglect, have also been shown to increase the risk of schizophrenia later in life.
Cannabis and Immigration: So, you mentioned the role of genetics, epigenetics, and inflammation. I’d like to mention the use of cannabis as a risk factor for developing psychosis as well, more specifically the THC component of cannabis. Something to keep in mind during these times when cannabis is being studied in more detail. Also, this is interesting: immigration puts you at risk for schizophrenia, and the risk can be as high as four-fold, depending on the study. Some explanations for this are increased discrimination, stress, and even low vitamin D. Tiffany, how do we diagnose schizophrenia?
DSM-5 Diagnostic Criteria:
The DSM-5 identifies 5 diagnostic criteria for schizophrenia:
- Patient must have two or more active phase symptoms for one month or longer: (1) Delusions, (2) Hallucinations (auditory, visual, or tactile) (3) Disorganized speech, (4) Negative symptoms (flat affect, avolition, social withdrawal, anhedonia), or (5) Catatonic behavior (which can be a collection of abnormal physical movements, the lack of movement or resistance to movement, psychomotor agitation). For the first criterion to be met, the patient must have delusions, hallucinations, or disorganized speech as one of their two presenting symptoms. Arreaza: The 1-month duration can be less if the patient is successfully treated.
- The symptoms experienced by the patient must impair their level of functioning in one or more major areas (professional career, relationships, and self-care). In addition, the disruption must be present most of the time since the onset of symptoms.
- There must be continuous signs of disturbance for at least 6 months. Within these 6 months, there must be at least 1 month where the patient experiences symptoms mentioned in the first criteria (delusions, hallucinations, disorganized speech, negative symptoms, or catatonic behavior). The disturbance may only be negative symptoms or attenuated positive symptoms (unusual perceptual experiences, odd beliefs, etc.)
- Mood disorders must be ruled out. This includes bipolar disorder with psychotic features, depressive disorder with psychotic features, and schizoaffective disorder.
- The behavioral disturbances must not be attributable to any substance use or medical conditions.
After the diagnosis of schizophrenia has been made for 1 year or more, specifiers can be added to further categorize the disease state, according to the DSM-V:
- Acute episode: a period in which all symptomatic criteria are met.
- Partial remission: a period in which symptomatic criteria are only partially met and symptoms are improved from a previous episode.
- Full remission: a period in which no symptomatic criteria are met (for a minimum of 6 months).
- Continuous: symptoms prevalent for the majority of the illness course.
Goals of Treatment:
- Reduce acute symptoms to allow patients to return to their baseline level of functioning.
- Prevent recurrence and maximize a patient’s quality of life using maintenance therapy.
There are 2 components of treatment: Pharmacotherapy and Psychosocial Intervention.
Pharmacotherapy.
Pharmacotherapy is initiated with second-generation antipsychotics as first-line agents due to their decreased risk of extrapyramidal side effects, compared to our first-generation antipsychotics. Commonly used medications include aripiprazole (Abilify), lurasidone (Latuda), risperidone (Risperdal), and quetiapine (Seroquel). These antipsychotics also have a more favorable side effect profile, showing a lower incidence of seizures, orthostatic hypotension, QT prolongation, weight gain, impaired glucose metabolism, and hyperlipidemia.
Of note, younger patients being treated for their first psychotic episode are more likely to experience metabolic side effects while on antipsychotics. Hence, it is important to start at lower doses in these patients and slowly titrate to a therapeutic dose.
Antipsychotics are implicated in the development of obesity, and obesity is one of my favorite topics. As a PCP, you need to have close communication with the psychiatrist before you change any doses of any antipsychotics, in my case, I just avoid making changes.
Older patients, who are likely on other medications should be started at doses that are ¼ to ½ the adult dose initially to monitor for any potential drug interactions. After therapy initiation, routine monitoring for symptomatic response is done weekly for the first 3 months. Signs of any extrapyramidal symptoms should also be evaluated at each visit.
Special care must be taken to patients with risk factors, for example, a metabolic profile should be ordered every 6 to 12 weeks depending on a patient’s comorbidities, and an EKG should be done before and 3 months after therapy initiation to monitor for QT prolongation.
QT prolongation is higher with ziprasidone, quetiapine, chlorpromazine, and intravenous (IV) haloperidol. Normal QTc intervals: Before puberty: NORMAL <450 ms, PROLONGED ≥460 ms. After puberty: Males, PROLONGED ≥470 ms. Females, PROLONGED ≥480 ms.
Duration of treatment.
APA guidelines state that if no or minimal response (= 20% improvement of symptoms) on 2 trials of antipsychotics for 2-4 weeks at an adequate dose or if a patient presents with a risk of suicide or aggressive behavior, not responsive to other treatments, a trial of clozapine is recommended. However, it is important to rule out secondary causes of medication unresponsiveness, such as non-compliance, and co-ingestion of other medications or substances, before initiation of clozapine.
For patients who struggle with compliance, long-acting antipsychotic injectables, which are given on a biweekly or monthly basis, may also be a more efficacious option before starting clozapine. Due to the rare but dangerous risk of agranulocytosis, absolute neutrophil levels must be monitored weekly for the first 6 months after treatment initiation of clozapine, then monthly thereafter.
Pharmacotherapy duration depends on the patient and the severity of symptoms. For example, the medication can be tapered off if the patient is experiencing their first episode and symptoms are minimally disruptive. However, in most cases, pharmacotherapy is often continued for at least 2-3 years, as maintenance, before tapering or discontinuation. Patients with severe, recurrent symptoms are typically kept on medications indefinitely due to higher risks of relapse.
Non-pharmacologic treatment.
Psychosocial interventions are focused on family intervention and therapy, social skills training, and cognitive behavioral therapy. Family intervention emphasizes providing support and education to the family/caretakers about the course of the disease, how to recognize symptoms, and understanding the importance of medication compliance. Trained and involved families/caretakers are associated with less frequent relapses, fewer hospital admissions, and less medication nonadherence.
Social skills training assists patients in learning basic skills to allow them to carry out everyday activities (taking a bus, paying bills, cooking). It is also used as a method to teach patients how to process emotions they perceive and emotions they experience. This allows patients the ability to build connections with those around them.
And finally, cognitive behavioral therapy, CBT, is often used to treat medication-resistant psychosis, to decrease the intensity of delusions or hallucinations. CBT focuses on guiding patients to challenge their delusions or hallucinations, by finding evidence that may negate what they see or hear.
In summary, schizophrenia is often seen as a chronic, debilitating condition with a nonlinear course and multifactorial etiology. However, with early diagnosis and a multidisciplinary treatment with consistent, longitudinal follow-up, patients have the potential to reach a functional and independent state in society. Patients who are treated promptly, ideally during their first episode of schizophrenia, have been shown to have a higher rate of remission and an overall better outcome. By understanding the complexity of schizophrenia and recognizing the barriers patients and caretakers may face, primary care physicians can provide the appropriate support, guidance, and resources.
_________________
Conclusion: Now we conclude episode number 170, “Schizophrenia Overview.” Future Dr. Chng explained that genetics, epigenetics, and inflammation are part of the causes of schizophrenia. She explained in detail the diagnostic criteria and how to start treatment. Dr. Arreaza also mentioned that cannabis and immigration can be risk factors for psychosis. Let’s keep in mind the antipsychotic medications, with their side effects and precautions, as part of the treatment, but let’s also remember the family and psychosocial interventions that impact the treatment of this disease.
This week we thank Hector Arreaza and Tiffanny Chng. Audio editing by Adrianne Silva.
Even without trying, every night you go to bed a little wiser. Thanks for listening to Rio Bravo qWeek Podcast. We want to hear from you, send us an email at [email protected], or visit our website riobravofmrp.org/qweek. See you next week!
_____________________
References:
- American Psychiatric Association. American Psychiatric Association Practice Guidelines for the Treatment of Psychiatric Disorders. Compendium 2006. American Psychiatric Association; 2006.
- Patel KR, Cherian J, Gohil K, Atkinson D. Schizophrenia: Overview and Treatment Options. P & T: a peer-reviewed Journal for Formulary Management. 2014;39(9):638-645. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4159061/
- Correll CU, Brieden A, Janetzky W. Symptomatic, functional and quality of life measures of remission in 194 outpatients with schizophrenia followed naturalistically in a 6-month, non-interventional study of aripiprazole once-monthly. Schizophrenia. 2023;9(1):1-8. doi: https://doi.org/10.1038/s41537-023-00405-5
- Jenkins TA. Perinatal complications and schizophrenia: involvement of the immune system. Frontiers in Neuroscience. 2013;7. doi: https://doi.org/10.3389/fnins.2013.00110
- National Institute of Mental Health. Schizophrenia. www.nimh.nih.gov. Published 2019. https://www.nimh.nih.gov/health/statistics/schizophrenia.
- Kadakia A, Catillon M, Fan Q, et al. The Economic Burden of Schizophrenia in the United States. The Journal of Clinical Psychiatry. 2022;83(6). doi: https://doi.org/10.4088/jcp.22m14458.
- Substance Abuse and Mental Health Services Administration. Impact of the DSM-IV to DSM-5 Changes on the National Survey on Drug Use and Health. Nih.gov. Published June 2016. https://www.ncbi.nlm.nih.gov/books/NBK519704/table/ch3.t22/.
- Royalty-free music used for this episode: Sur La Tabla Beat by audiohero, downloaded on July 20, 2023, from https://www.videvo.net/royalty-free-music.
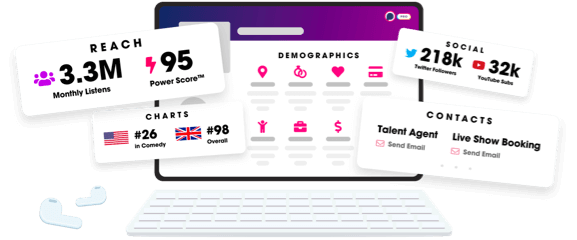
Join Podchaser to...
- Rate podcasts and episodes
- Follow podcasts and creators
- Create podcast and episode lists
- & much more
Episode Tags
Claim and edit this page to your liking.
Unlock more with Podchaser Pro
- Audience Insights
- Contact Information
- Demographics
- Charts
- Sponsor History
- and More!
- Account
- Register
- Log In
- Find Friends
- Resources
- Help Center
- Blog
- API
Podchaser is the ultimate destination for podcast data, search, and discovery. Learn More
- © 2024 Podchaser, Inc.
- Privacy Policy
- Terms of Service
- Contact Us
