In this week's episode of the Spine & Nerve podcast, Drs. Nicolas Karvelas and Brian Joves discuss infectious spondylodiscitis, a relatively rare inflammatory process involving an intervertebral disc and the adjacent vertebral bodies.
Spondylodiscitis has a prevalence of about 4-24 per million, and has been increasing as patients have more risk factors (advanced age, immunocompromised states such as HIV infection, intravenous drug users, healthcare-associated infections, expansion of spinal surgery indications) and improved diagnostic modalities.
Patients generally present with pain and tenderness in the region, about 50% present with high fever, and about 1/4 with neurologic compromise. The symptoms can be fairly non-specific, so patients with risk factors must be evaluated with a high degree of suspicion.
Infection is the most common cause of spondylodiscitis, which is often spontaneous and hematogenous in origin and most commonly affects the lumbar spine, followed by thoracic, cervical, and sacral. The infectious pathogens can be pyogenic (bacterial), granulomatous (tuberculosis, fungal), or parasitic, though many noninfectious processes affecting the spine such as pseudarthrosis in ankylosing spondylitis, amyloidosis, destructive spondyloarthropathy of hemodialysis, Modic changes type 1, neuropathic arthropathy, calcium pyrophosphate dehydrate (CPPD) spondyloarthropathy and gout can mimic infectious discitis/ osteomyelitis.
To determine whether a particular patient’s spinal process is due to an infectious versus non-infectious cause and to determine the pathogencan be challenging. Clinical findings and laboratory studies including erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) can be helpful in the diagnosis due to their high sensitivity; however, their specificity is low. Magnetic resonance imaging and biopsy have become the standard when working up this process, particularly in cases where the origin of the pathogen is unknown.
Listen as the doctors give a high-level overview of this disease process, and walk us through the challenging diagnostic process of a disease that may have an insidious onset, with subtle and misleading clinical features and briefly discuss management requiring a multidisciplinary approach involving radiologists, infectious diseases specialists, spine surgeons and rehabilitation personnel.
This podcast is for information and educational purposes only, it is not meant to be medical or career advice. If anything discussed may pertain to you, please seek council with your healthcare provider. The views expressed are those of the individuals expressing them, they may not represent the views of Spine & Nerve.
1. Salaffi, F., Ceccarelli, L., Carotti, M. et al. Differentiation between infectious spondylodiscitis versus inflammatory or degenerative spinal changes: How can magnetic resonance imaging help the clinician?. Radiol med 126, 843–859 (2021).
2. Mavrogenis AF, Megaloikonomos PD, Igoumenou VG, et al. Spondylodiscitis revisited. EFORT Open Rev. 2017;2(11):447-461. Published 2017 Nov 15. doi:10.1302/2058-5241.2.160062
From The Podcast
Spine & Nerve
We are physicians who practice pain management and physical medicine and rehabilitation, and believe that the main goal of practice is to improve the quality of life of our patients and communities. We will dive deep into the world of modern pain management to help healthcare providers and consumers understand various diagnoses, treatment options, and the changing landscape of pain management.This podcast is meant for educational and entertainment purposes only, and is not medical advice.Join Podchaser to...
- Rate podcasts and episodes
- Follow podcasts and creators
- Create podcast and episode lists
- & much more
Episode Tags
Claim and edit this page to your liking.
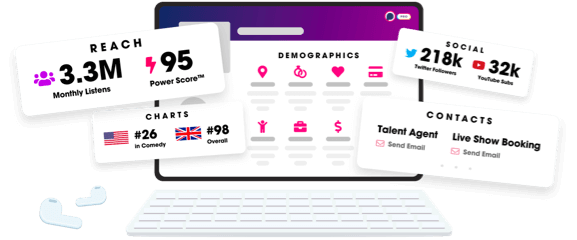
Unlock more with Podchaser Pro
- Audience Insights
- Contact Information
- Demographics
- Charts
- Sponsor History
- and More!
- Account
- Register
- Log In
- Find Friends
- Resources
- Help Center
- Blog
- API
Podchaser is the ultimate destination for podcast data, search, and discovery. Learn More
- © 2024 Podchaser, Inc.
- Privacy Policy
- Terms of Service
- Contact Us
